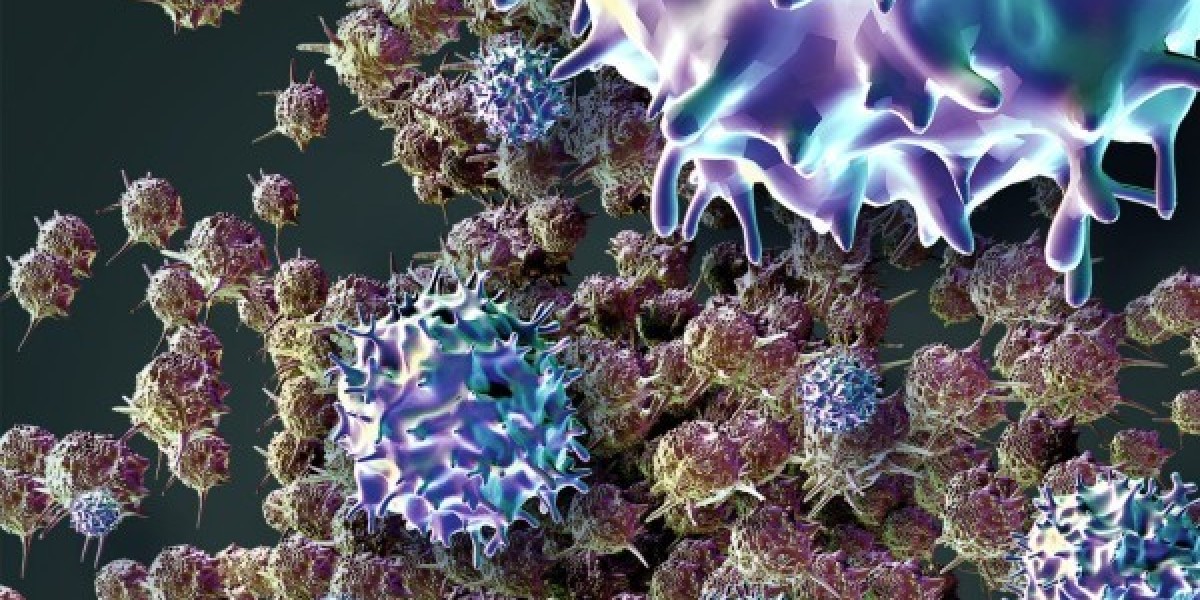
Adoptive cell therapy is a type of immunotherapy that involves extracting immune cells from a patient or donor and modifying them in the laboratory before transfusing them back into the patient. The goal of this therapy is to harness the power of the patient’s own immune system or donor cells to fight cancer. This therapy has shown promise in treating several types of cancer including hematological cancers like leukemia and lymphoma as well as some solid tumors like melanoma.
How It Works ?
In adoptive cell therapy, immune cells called T cells are extracted from a patient or donor using a process called leukapheresis. These T cells are then grown and modified in the lab before being transfused back into the patient. There are two main types of cells used in this therapy - tumor infiltrating lymphocytes (TILs) and chimeric antigen receptor (CAR) T cells.
Adoptive Cell Therapy involves extracting immune cells from a patient’s own tumor. These T cells have already shown an ability to recognize and attack cancer cells. In the lab, they are grown in large quantities and activated to more effectively fight cancer. They are then given back to the patient to boost their immune response.
CAR T cell therapy involves engineering a patient's T cells to specifically target antigens on tumor cells. The genes of the T cells are modified using a virus to introduce a chimeric antigen receptor (CAR) that programs the T cells to attack the cancer. The CAR redirects the T cells to target the antigen and triggers their activation once bound to the cancer cell. This enhances their ability to find and destroy cancer cells in the body.
Potential of CAR T Cell Therapy
CAR T cell therapy has shown great promise in treating certain blood cancers where the antigen target is well-defined. In clinical trials, it has achieved complete remission rates of 70-90% in adult patients with acute lymphoblastic leukemia (ALL) that was refractory or in relapse. For lymphoma, complete response rates of 55-76% have been observed.
Novartis' Kymriah became the first CAR T cell therapy approved by the FDA in 2017 for the treatment of ALL in pediatric and young adult patients. The approval was based on trials showing 83% of patients achieving complete remission. Additional CAR T cell therapies have since been approved for blood cancers.
Research is ongoing to expand the use of CAR T cell therapy to treat solid tumors. However, this poses significant challenges since solid tumors tend to be more heterogeneous with multiple tumor antigens. Finding suitable targets and enhancing T cell persistence in the solid tumor microenvironment will be important for success. Some early trials for cancers like glioblastoma and pancreatic cancer have shown encouraging responses.
Managing Side Effects of Adoptive Cell Therapy
While highly effective, adoptive cell therapies can also cause severe side effects due to the highly activated T cells circulating throughout the body. Common side effects observed include cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS).
CRS occurs when large numbers of activated T cells flood the bloodstream and release inflammatory cytokines. This can cause high fevers, low blood pressure, respiratory issues and even life-threatening events in rare cases. ICANS is associated with CRS and causes confusion, changes in mental status or seizures due to the effects of inflammatory cytokines on the brain.
Careful patient selection and risk mitigation strategies are important. Doses are often administered in the hospital so side effects can be identified and treated immediately. Steroids like dexamethasone are the main treatment for CRS and ICANS. As experience with these therapies increases, side effect management continues to improve.
Future Outlook and Hurdles
Adoptive cell therapy has come a long way from early promising results to FDA-approved therapies available today. Continued research aims to overcome remaining hurdles and fully realize the potential of these ‘living drugs’. Key future directions include improving T cell engineering techniques, developing predictors of response, combining with other immunotherapies, and overcoming immunosuppression in the tumor microenvironment.
Manufacturing challenges need solutions to produce cell therapies in a more affordable and scalable manner. Toxicity management will be refined as more patient data accumulates. Clinical testing also needs to expand use to additional cancer types. Overall, with ongoing advances, adoptive cell therapy may broaden immunotherapy options for many patients with different cancer types in the years ahead.
Get more insights on Adoptive Cell Therapy